User:MrBugsyBubz/Inactivated vaccine
| This is the sandbox page where you will draft your initial Wikipedia contribution.
If you're starting a new article, you can develop it here until it's ready to go live. If you're working on improvements to an existing article, copy only one section at a time of the article to this sandbox to work on, and be sure to use an edit summary linking to the article you copied from. Do not copy over the entire article. You can find additional instructions here. Remember to save your work regularly using the "Publish page" button. (It just means 'save'; it will still be in the sandbox.) You can add bold formatting to your additions to differentiate them from existing content. |
Article Draft[edit]
Lead[edit]
| MrBugsyBubz/Inactivated vaccine | |
|---|---|
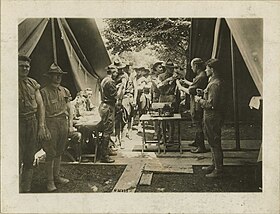 Typhoid prophylaxis for soldiers in World War I. | |
| Other names | Killed vaccine |
| Specialty | Public health, Immunology, Family medicine, General practice |
| Uses | prevention of infectious diseases |
| Frequency | birth to adulthood |
| Outcomes | development of active immunity in individuals; contribution to herd immunity |
An inactivated vaccine (or killed vaccine) is a vaccine consisting of virus particles, bacteria, or other pathogens that have been grown in culture and then killed to destroy disease producing capacity. In contrast, live vaccines use pathogens that are still alive (but are almost always attenuated, that is, weakened). Pathogens for inactivated vaccines are grown under controlled conditions and are killed as a means to reduce infectivity and thus prevent infection from the vaccine.[1]
Inactivated vaccines were first developed in the late 1800s and early 1900s for cholera, plague, and typhoid.[2] Today, inactivated vaccines exist for many pathogens, including influenza, polio (IPV), rabies, hepatitis A and pertussis.[3]
Because inactivated viruses tend to produce a weaker response by the immune system than live viruses, immunologic adjuvants and multiple "booster" injections may be required in some vaccines to provide an effective immune response against the pathogen.[1][4][5] Attenuated vaccines are often preferable for generally healthy people because a single dose is often safe and very effective. However, some people cannot take attenuated vaccines because the pathogen poses too much risk for them (for example, elderly people or people with immunodeficiency). For those patients, an inactivated vaccine can provide protection.
Article body[edit]
Mechanism[edit]
The pathogen particles are destroyed and cannot divide, but the pathogens maintain some of their integrity to be recognized by the immune system and evoke an adaptive immune response.[6][7] When manufactured correctly, the vaccine is not infectious, but improper inactivation can result in intact and infectious particles.[citation needed]
When a vaccine is administered, the antigen will be taken up by an antigen-presenting cell and transported to a draining lymph node in vaccinated people. The APC will place a piece of the antigen, an epitope, on its surface along with a major histocompatibility complex (MHC) molecule. It can now interact with and activate T cells. The resulting helper T cells will then stimulate an antibody-mediated or cell-mediated immune response and develop an antigen-specific adaptive response.[8][9] This process creates an immunological memory against the specific pathogen and allows the immune system to respond more effectively and rapidly after subsequent encounters with that pathogen.[6][8][9]
Inactivated vaccines tend to produce an immune response that is primarily antibody-mediated.[3][10] However, deliberate adjuvant selection allows inactivated vaccines to stimulate a more robust cell-mediated immune response.[1][7]
Types[edit]
Inactivated vaccines often refer to non-live vaccines.[3][8] They are further classified depending on the method used to inactivate the pathogen:[3][4]
- Whole pathogen inactivated vaccines are produced when an entire pathogen is 'killed' using heat, chemicals, or radiation,[5] although only formaldehyde and beta-Propiolactone exposure are widely used in human vaccines.[11]
- Subunit vaccines are produced by purifying out the antigens that best stimulate the immune system to mount a response to the virus, while removing other components necessary for the virus to replicate or survive or that can cause adverse reactions.[4][5]
- Split virus vaccines are produced by using a detergent to disrupt the viral envelope.[4][12] This technique is used in the development of many influenza vaccines.[13]
- Toxoid vaccines are created by inactivating toxins produced by bacteria.[3][14] The toxoid mounts an immune response against the toxin.[15]
Examples[edit]
Types include:[16]
- Viral:
- Bacterial:
Advantages and disadvantages[edit]
Advantages[edit]
- Inactivated pathogens are more stable than live pathogens. Increased stability facilitates the storage and transport of inactivated vaccines.[8][15][17]
- Unlike live attenuated vaccines, inactivated vaccines cannot revert to a virulent form and cause disease.[6][10] For example, there have been rare instances of the live attenuated form of poliovirus present in the oral polio vaccine (OPV) becoming virulent, leading to the inactivated polio vaccine (IPV) replacing OPV in many countries with controlled wild-type polio transmission.[6][9]
- Unlike live attenuated vaccines, inactivated vaccines do not replicate and are not contraindicated for immunocompromised individuals.[6][7][8]
Disadvantages[edit]
- Inactivated vaccines have a reduced ability to produce a robust immune response for long-lasting immunity when compared to live attenuated vaccines.[3]
- Subunit vaccines have reduced immunogenicity compared to inactivated whole-pathogen vaccines.[9]
- Adjuvants and boosters are often required to produce and maintain protective immunity.[15][10]
- Pathogens must be cultured and inactivated for the creation of killed whole-organism vaccines.[6][9] This process slows down vaccine production when compared to genetic vaccines.[8]
References[edit]
- ^ a b c Petrovsky, Nikolai; Aguilar, Julio César (2004-09-28). "Vaccine adjuvants: Current state and future trends". Immunology and Cell Biology. 82 (5): 488–496. doi:10.1111/j.0818-9641.2004.01272.x. ISSN 0818-9641. PMID 15479434. S2CID 154670.
- ^ Plotkin, Stanley A.; Plotkin, Susan L. (2011). "The development of vaccines: how the past led to the future". Nature Reviews Microbiology. 9 (published 2011-10-03): 889–893. doi:10.1038/nrmicro2668. ISSN 1740-1534. PMID 21963800. S2CID 32506969.
- ^ a b c d e f Centers for Disease Control and Prevention (2021). "Chapter 1: Principles of Vaccination" (PDF). In Hall, Elisha; Wodi, A. Patricia; Hamborsky, Jennifer; Morelli, Valerie; Schilllie, Sarah (eds.). Epidemiology and Prevention of Vaccine-Preventable Diseases (14th ed.). Washington, D.C.: Public Health Foundation.
- ^ a b c d WHO Expert Committee on Biological Standardization (19 June 2019). "Influenza". World Health Organization (WHO). Retrieved 22 October 2021.
- ^ a b c "Types of Vaccines". Vaccines.gov. U.S. Department of Health and Human Services. 23 July 2013. Archived from the original on 9 June 2013. Retrieved 16 May 2016.
- ^ a b c d e f Vetter, Volker; Denizer, Gülhan; Friedland, Leonard R.; Krishnan, Jyothsna; Shapiro, Marla (2018-02-17). "Understanding modern-day vaccines: what you need to know". Annals of Medicine. 50 (2): 110–120. doi:10.1080/07853890.2017.1407035. ISSN 0785-3890. PMID 29172780. S2CID 25514266.
- ^ a b c Slifka, Mark K.; Amanna, Ian (2014-05-23). "How advances in immunology provide insight into improving vaccine efficacy". Vaccine. 32 (25): 2948–2957. doi:10.1016/j.vaccine.2014.03.078. ISSN 0264-410X. PMC 4096845. PMID 24709587.
- ^ a b c d e f Pollard, Andrew J.; Bijker, Else M. (2020-12-22). "A guide to vaccinology: from basic principles to new developments". Nature Reviews. Immunology: 1–18. doi:10.1038/s41577-020-00479-7. ISSN 1474-1733. PMC 7754704. PMID 33353987.
- ^ a b c d e Karch, Christopher P.; Burkhard, Peter (2016-11-15). "Vaccine technologies: From whole organisms to rationally designed protein assemblies". Biochemical Pharmacology. 120: 1–14. doi:10.1016/j.bcp.2016.05.001. ISSN 0006-2952. PMC 5079805. PMID 27157411.
- ^ a b c Plotkin, Stanley A.; Orenstein, Walter A.; Offit, Paul A., eds. (2018). "Technologies for Making New Vaccines". Plotkin's vaccines (7th ed.). Philadelphia, PA: Elsevier. ISBN 978-0-323-39302-7. OCLC 989157433.
- ^ Sanders, Barbara; Koldijk, Martin; Schuitemaker, Hanneke (2015). "Inactivated Viral Vaccines". Vaccine Analysis: Strategies, Principles, and Control: 45–80. doi:10.1007/978-3-662-45024-6_2. ISBN 978-3-662-45023-9. S2CID 81212732.
- ^ Chen, Jidang; Wang, Jiehuang; Zhang, Jipei; Ly, Hinh (2021). "Advances in Development and Application of Influenza Vaccines". Frontiers in Immunology. 12: 2740. doi:10.3389/fimmu.2021.711997. ISSN 1664-3224. PMC 8313855. PMID 34326849.
{{cite journal}}: CS1 maint: PMC format (link) CS1 maint: unflagged free DOI (link) - ^ National Advisory Committee on Immunization (NACI) (May 2018). NACI literature review on the comparative effectiveness and immunogenicity of subunit and split virus inactivated influenza vaccines in adults 65 years of age and older (PDF). ISBN 9780660264387. Cat.: HP40-213/2018E-PDF; Pub.: 180039.
{{cite book}}:|website=ignored (help); Unknown parameter|lay-url=ignored (help) - ^ "Toxoid vaccines - WHO Vaccine Safety Basics". vaccine-safety-training.org. World Health Organization (WHO). Retrieved 2021-11-15.
{{cite web}}: CS1 maint: url-status (link) - ^ a b c Clem, Angela S (2011). "Fundamentals of Vaccine Immunology". Journal of Global Infectious Diseases. 3 (1): 73–78. doi:10.4103/0974-777X.77299. ISSN 0974-777X. PMC 3068582. PMID 21572612.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Immunization". Retrieved 2009-03-10.
- ^ "Inactivated whole-cell (killed antigen) vaccines - WHO Vaccine Safety Basics". vaccine-safety-training.org. World Health Organization (WHO). Retrieved 2021-11-11.
{{cite web}}: CS1 maint: url-status (link)
