User:Mr. Ibrahem/X-linked agammaglobulinemia
| X-linked agammaglobulinemia | |
|---|---|
| Other names | Bruton agammaglobulinemia, Btk agammaglobulinemia, Bruton tyrosine kinase agammaglobulinemia, agammaglobulinemia of Bruton, congenital agammaglobulinemia, X-linked hypogammaglobulinemia, Bruton type agammaglobulinemia, Bruton syndrome, sex-linked agammaglobulinemia[1][2] |
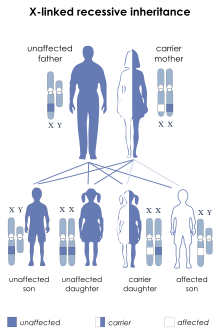 | |
| The disorder is passed on in an X-linked recessive pattern | |
| Specialty | Medical genetics |
| Symptoms | No tonsils, recurrent bacterial infections[3][4] |
| Complications | Bronchiectasis, cancer[4] |
| Usual onset | 6 months of age[3] |
| Causes | Mutation of the Btk gene[3] |
| Diagnostic method | Low immunoglobulins and B cells, genetic testing[4] |
| Differential diagnosis | Autosomal recessive agammaglobulinemia, autosomal dominant agammaglobulinemia, common variable immunodeficiency, hyper IgM syndrome, combined immunodeficiency[3] |
| Treatment | Immunoglobulin therapy, antibiotics, vaccination[3] |
| Frequency | 1 in 100,000 newborn males[1] |
X-linked agammaglobulinemia (XLA) is a genetic disorder that affects the body's ability to fight infection.[1] Those affected typically present around 6 months of age with recurrent bacterial infections including pneumonia, middle ear infections, cellulitis, diarrhea, and conjunctivitis.[3] Other symptoms include a lack of tonsils and no lymph nodes.[4] Complications can include bronchiectasis and cancer.[4]
Its is caused by various mutations of the Bruton's tyrosine kinase (Btk) gene and is inherited in an X-linked recessive manner.[3][1] The underlying mechanism involves an inability to form mature B cells, and thus the inability to make antibodies.[4] It is a type of primary immunodeficiency disorder.[4] Diagnosis is usually based on low immunoglobulins and B cells in the blood and can be confirmed by genetic testing.[4]
There is no cure.[1] Treatment is generally with immunoglobulin therapy either through a vein (IVIG) or subcutaneously (SCIG).[3] When infections do occur, longer courses of antibiotics are generally required.[3] Long-term antibiotics may also be used to try to prevent infections.[3] Those affected should receive all vaccines except live vaccines.[3][1] Treatment is required for survival and with treatment survival is generally beyond the age of 40.[1]
XLA affects about 1 in 100,000 live newborn males.[1] It was described by Ogden Bruton in 1952 and was the first known primary immunodeficiency disorder.[5][6] Effective treatment became available in the 1970s; however, is often costly.[1]
References[edit]
- ^ a b c d e f g h i Lackey, AE; Ahmad, F (January 2020). "X-linked Agammaglobulinemia". PMID 31751055.
{{cite journal}}: Cite journal requires|journal=(help) - ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. p. 83. ISBN 0-7216-2921-0.
- ^ a b c d e f g h i j k "X-linked agammaglobulinemia | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Archived from the original on 30 January 2021. Retrieved 28 January 2021.
- ^ a b c d e f g h "X-linked Agammaglobulinemia - Immunology; Allergic Disorders". Merck Manuals Professional Edition. Archived from the original on 30 July 2020. Retrieved 28 January 2021.
- ^ Bruton OC (1952). "Agammaglobulinemia". Pediatrics. 9 (6): 722–8. PMID 14929630.. Reproduced in Buckley CR (1998). "Agammaglobulinemia, by Col. Ogden C. Bruton, MC, USA, Pediatrics, 1952;9:722-728". Pediatrics. 102 (1 Pt 2): 213–5. PMID 9651432.
- ^ Mahdaviani, Seyed Alireza; Rezaei, Nima (2018). Pulmonary Manifestations of Primary Immunodeficiency Diseases. Springer. p. 78. ISBN 978-3-030-00880-2. Archived from the original on 2021-08-27. Retrieved 2021-01-28.
