Talk:Toothache/Archive 1
| This is an archive of past discussions. Do not edit the contents of this page. If you wish to start a new discussion or revive an old one, please do so on the current talk page. |
| Archive 1 | Archive 2 |
Untitled
It submitted my edit before I could explain...basically, someone deleted most of a paragraph of unreferenced medical advice. They left only a couple of sentences, which talk about the deleted information, so that you need the deleted information to understand what the remaining part is talking about. -- 12.116.162.162 18:57, 18 April 2007 (UTC)
clarification on previous sentence
Lesion - what did you mean by
The tooth pulp behaves like a visceral structure in terms of how associated pain is perceived.[1]
I'm not sure how to use the reference Ian Furst (talk) 14:06, 20 December 2013 (UTC)
- This is expansion of the observation that isolated pulpal pain is usually poorly localized. The pulp lacks proprioceptors and only has nocioceptors. Visceral pain is poorly localized, compared to say hitting your hand with a hammer, in which the pain is well localized. Testicular pain is also visceral, it is felt deep in the pelvis/stomach, because embryologically testes begin as intrapelvic organs. Lesion (talk) 14:21, 20 December 2013 (UTC)
headings odontogenic/non-odontogenic
Lesion; I was still going to discuss odontogenic and non-odontogenic classification, but the individual headings add almost nothing except maybe to the dental audience. Should we just ditch the extra headings? Ian Furst (talk) 15:08, 20 December 2013 (UTC)
- It is difficult. We are not writing a patient information leaflet, and neither are we writing a essay for medical professionals. We need to be encyclopedic in our coverage of the topic, but it needs to be readily understandable and have all jargon explained for a general audience. Happy to discuss ... what layout of headings do you suggest instead? Lesion (talk) 15:15, 20 December 2013 (UTC)
- Also, do you think that "dental toothache" in brackets or instead of odontogenic, as with "non-dental toothache" instead of non-odontogenic; might be more understandable for readers? Lesion (talk) 15:21, 20 December 2013 (UTC)
- think you've got the right wording with Dental causes of toothach and Non-dental causes of toothache. Reworded, I think they're better in as heading groups. Ian Furst (talk) 15:55, 20 December 2013 (UTC)
- Along the same lines, maybe we should change pulpal and periodontal to "Tooth" and "Supporting structures". Then the rest can stay with proper headings? Just trying to think like the general reader. Ian Furst (talk) 15:58, 20 December 2013 (UTC)
- think you've got the right wording with Dental causes of toothach and Non-dental causes of toothache. Reworded, I think they're better in as heading groups. Ian Furst (talk) 15:55, 20 December 2013 (UTC)
- OK I changed the headings to dental / non-dental.
- Not sure about tooth/supporting structures... "tooth" is a bit ambiguous compared to pulpal imo... This article could benefit form a very brief section explaining basic dental anatomy. I see you have started to do this in the pulpitis section. Perhaps this should be moved to "definitions"? I was also wondering if we should move "pathophysiology" to before "differential diagnosis"?
- The article is such a state it is hard to know where to start...
- If I understand you correctly, you propose to remove subheadings like "pulpitis", "dentin hypersensitivity" and just have 2 long "pulpal" and "periodontal" sections ... I am also not sure about this. With subheadings, there is an obvious layout for the different individual causes, and also we emphasize that we have main articles for each of these causes... It might look better once the other subsections are expanded. Suggest we wait and see what that looks like? Lesion (talk) 18:19, 20 December 2013 (UTC)
I see you have merged the other "pulpal" causes of toothache into a section called "pulpitis". I question whether dentin hypersensitivity is a type of pulpitis. If these are merged (which I think is less clear for readers), then the title has to be something wider than pulpitis for accuracy. Lesion (talk) 21:05, 20 December 2013 (UTC)
- Just going thru the other comments above (8's and an icestorm today - never a dull moment):
- Totally agree on putting a short anatomy lesson into the definition section. Maybe we make a small diagram as well.
- I always thought hypersensitivity was just a mild variant of pulpitis, but I can check into it unless you're positive (I haven't read on the subject in years). I've emailed a couple of endo friends to ask.
- Re the merging of sections; my logic was that I'm not a fan of creating sections for 1 or 2 sentences especially when they have their own article. In this case, both dent hyper and cracked tooth syndrome had their own article and very limited info under the pulpitis area. Thought it was more readable keeping it in the narrative then adding the wikilinks and less "textbook" like in the classification, given what I believed to be similar pathophysiology.
- I had no intention of doing the same to periodontal a) didn't want to overwrite something you'd been working on b) because the causes of periodontal are based on different anatomic structures and pathophysiology, the subheadings work well imo.
- Re the section order, as I started to look at the rest of the article, it seems like a lot of them won't work well within the context of the set-up. Personally, I think we need to throw the recommendation of MEDMOS out the window in this regard. There's little value to adding a heading for treatment only to say it varies by cause. Whereas the diagnostic approach section should be an amazing discussion about how easy it is to miss diagnose, sensitivities, etc... Pathophysiology, really get's dealt with in the differential diagnosis section. Why don't we build the sections that flow well, leave the less used ones in for now, then revisit the issue as we go?
- re thumbnail size. That pink tooth pic looks way out of proportion in the paragraph. What's the rationale behind leaving them as thumbnail? Doesn't balance esthetically. Should we just take it out?
Ian Furst (talk) 23:21, 20 December 2013 (UTC)
Replies:
- OK
- I am not sure about this. Dentin hypersensitivity might simply represent decreased insulation for the pulp, and does not necessarily imply any pulpal inflammation. I will take a hiatus from working on this page to expand dentin hypersensitivity so I will understand this facet of the main topic better.
- The subsections were currently one or 2 sentences. I anticipated they would grow in length to a few short paragraphs each.
- If pulpal is to be discussed as a narrative, it makes sense to also discuss all periodontal causes as a narrative. I would not mix and match. Imo, depends if all "pulpal" causes can be lumped under the heading "pulpitis" or not.
- MEDMOS is a guide only. If it is not readily applicable to this topic we should not hesitate to adapt it. Pathophysiology section currently contains some random content. I also have difficulty in distinguishing this section from "causes" in other articles. Tend to merge them together. Perhaps pathophysiology should discuss innervation, different types of pain fibres in pulp and periodontium, and overall picture of how many of the dental causes progress from one stage to the next. On the other hand, it could potentially all be dealt with in differential diagnosis.
- I was looking in the MOS about this. Then I quickly remembered again why I never read that thing. It basically says, use thumbnail unless there is some reason not to, so this is fine. Generally people tend to change non thumbnail size images to thumb however. Lesion (talk) 00:15, 21 December 2013 (UTC)
Li2011
I took Li2011 out of a reference in the pulpal area (switching over to non-primary) - but you'd used it in the perio section, sorry. Do you have the original reference or do you mind if I replace the refrence with one from pathways of the pulp (non-primary)? Ian Furst (talk) 14:02, 22 December 2013 (UTC)
which section is next
any preference for which section I hit next? Ian Furst (talk) 17:18, 23 December 2013 (UTC)
- Up to you... there is much to do... I was going to continue on cracked tooth syndrome and then suggest the wording of that section. Lesion (talk) 17:21, 23 December 2013 (UTC)
Non-dental toothache section
I have tweaked the wording here. Also I feel we have a problem with this sentence:
- "pain can be psychogenic in origin as in the case of Munchausen's syndrome or drug seeking behavior"
Terms like psychogenic, somatoform and psychosomatic are commonly misused, but they have different definitions.
- Psychogenic pain is real pain. Patients will actually experience real pain. This is very rare.
- Munchausen patients are not in pain, they know they are not in pain. The defining feature of this condition is that symptoms are invented by the patient for whatever reason. This is not psychogenic pain.
Similarly, there is difficultly linking psychogenic pain with drug seeking behavior...
There is a minefield of psych terms which we should probably avoid as much as possible... least of all because they keep changing the names of everything... Suggest if we are going to use any psych term, we keep it very general, not naming any specific condition like Munchausen, and make sure we give a correct definition. Lesion (talk) 18:50, 23 December 2013 (UTC)
In terms of organic disease, I do not think we mention enough ... TMD? Although perhaps we will discuss that more in the section "occlusal trauma". I'm guessing that overloading of the periodontal ligament is the main mechanism by which TMD and bruxism cause dental pain. We also don't mention maxillary sinusitis... Suggest we start a list of things we want to cover here: Lesion (talk) 14:25, 25 December 2013 (UTC)
pictures sizes
the esthetics and balance of the thumb size pics are making me apeshit. I'm going to resize them, for now, and recalibrate the originals down the road. Hope that's ok Ian Furst (talk) 14:07, 22 December 2013 (UTC)
- Apparently MOS says generally use thumbnail unless there is a specific reason not to, like in this case that thumbnail is not the ideal size. Lesion (talk) 16:08, 22 December 2013 (UTC)
- While we are talking about images, is there a better version of this image that you are aware of? Lesion (talk) 22:21, 22 December 2013 (UTC)
- didn't really look. will watch for one.Ian Furst (talk) 22:44, 22 December 2013 (UTC)
- can't find one, will take a 1/2 decent tooth pic and add tubules. Ian Furst (talk) 23:31, 22 December 2013 (UTC)
- updated an existing photo in commons with dentin tubules and labels, about as good as I can do. Ian Furst (talk) 02:21, 23 December 2013 (UTC)
- While we are talking about images, is there a better version of this image that you are aware of? Lesion (talk) 22:21, 22 December 2013 (UTC)
- What am I talking about, we already had Tooth section.svg ... Which is better? I prefer the colors and minimal annotations on Basic anatomy tooth.jpg, but I don't like the way the root apices fade off... Thoughts? Lesion (talk) 03:10, 23 December 2013 (UTC)
- fine with tooth section.svg, but when you explode it, because it lacks a white background (or any background as an .svg), the labels are lost in the viewers black background. Needs to be turned into .jpg or white background added, I'll also add dentin tubules, didn't link that the dentin looks solid Ian Furst (talk) 12:53, 23 December 2013 (UTC)
- What am I talking about, we already had Tooth section.svg ... Which is better? I prefer the colors and minimal annotations on Basic anatomy tooth.jpg, but I don't like the way the root apices fade off... Thoughts? Lesion (talk) 03:10, 23 December 2013 (UTC)
what's that? Ian Furst (talk) 16:55, 23 December 2013 (UTC)
- Update: user:Goran tek-en is making a great new diagram for dental anatomy and related dental pathology articles. This article is not the only one which would benefit from this new diagram, so when the new diagram is ready it would be good to update older versions on other articles too. Lesion (talk) 22:17, 28 December 2013 (UTC)
dentin hypersensitivity
Also posted on talk:dentin hypersensitivity
Pathophysiology theories
Hey Lesion, received a response back from an endo colleague regarding the etiology of the pain after asking if it was a mild pulpitis,
| “ | No ! Dentinal sensitivity is the branstrom theory of fluid movement inside the Dentinal tubules and that causes firing if the nerves ending in the outer layer of the pulp. Theoricly[sic] pulp is healthy. Now repetitive and constant stimulus can be etiology for a future pulpitis. Check.[sic] Bramstron | ” |
| — S.Abitbol, Endodontist, email communications | ||
With that info, I found a review at pubmed pmid 22238734.
Bottom line, I think is that it's got to be it's own subcat, and by the same logic so does cracked tooth pain. Will modify both. Ian Furst (talk) 11:33, 21 December 2013 (UTC)
- Responded on talk:dentin hypersensitivity. I've worked a bit on that article. It is not perfect, but at least all the advertising and primary sources are gone. Few Qs at this point:
- How much detail should we go into for each cause of toothache? I was reading it through again today and I thought perhaps that the periodontal abscess section is too long? The major causes such as pulpitis deserve greater coverage imo, but the rarer conditions might only need a short para each... Lesion (talk) 16:55, 22 December 2013 (UTC)
- What is the pathophysiology section doing? Should we move it to before the differential diagnosis section? It could then include the short intro to basic dental anatomy that we were talking about earlier...
- I added the line "Cracked tooth syndrome is a special type of pulpitis" with no reference before ... again now I think we need to question this... but I don't know enough about the topic. Had a look at cracked tooth syndrome but currently it doesn't help us much. It says "untreated it can progress to severe pain, pulp death and even loss of the tooth." I suppose a superficial crack into dentin might cause dentin hyypersensitivty with no significant pulpitis, but a deeper crack into the pulp would likely cause pulpitis. I'll do some quick work on that page so we can generate easily some short content for toothache. Lesion (talk) 16:55, 22 December 2013 (UTC)
Proposed wording of dentin hypersensitivity content
Here is a brief summary of the content on dentin hypersensitivty. I will put inline refs in later, they can be easily re-used from that article. Lesion (talk) 16:55, 22 December 2013 (UTC)
Dentin hypersensitivity (also termed dentin sensitivity) is a very common cause of dental pain, occurring in about 15% of the general population to some degree. The pain is short lasting and sharp in character. It is triggered by thermal stimulae, especially cold drinks or cold air; or mechanical contact, e.g. toothbrushing. The main cause of dentin hypersensitivity is exposed dentin, which is normally covered by enamel or cementum and gingiva. A common scenario is gingival recession (receding gums) caused by either long term forceful/excessive toothbrushing or chronic periodontitis (gum disease). Being softer than enamel, the cementum and dentin are vulnerable to tooth wear (e.g. acid erosion caused by frequent consumption of acidic foods and drinks or conditions such as gastroesophageal reflux disease; or abrasion from toothbrushing). When dentin is exposed, dentinal tubules permit temperature and osmotic changes to be more readily detected by the nerves in the pulp. It is thought that dentin hypersensitivity usually represents a healthy, non-inflamed pulp responding to a lack of insulating layers of dental hard tissues to protect it from the external environment. There are many treatments and preventative strategies for dentin hypersensitivity, including desensitizing toothpastes and protective varnishes which are applied to the exposed dentin surface.
- 1. looks good, I was (literally) just reading up on this. The reference from 10th POP is {{cite isbn|9780323064897|pages=478-481}}
- 2. I think it's worthwhile to mention the hydrodynamic mechanism of dentin sensitivity by name
- 3. For the layperson, the opening of the paragraph fails to provide context wrt dentin. I would make the tie earlier on to "sensitive teeth">>exposed roots>>exposed dentin>>pain. I was going to create a paragraph something like:
Sensitive teeth, or dentin hypersensitivity, is the short lasting pain to stimulants like cold drinks and spicy foods that occurs in 15% of the population. The pain is caused by a complex mechanism where the roots of teeth become exposed (often from GERD or abrasion) and the dentin of the root is laid bare to the mouth. Dentin, has small tubules which hold fluid and communicate with the pulp of the tooth. The pulp, in turn, has mechanotransducers, small nerve bodies that translate the movement of fluid into nerve impulses in the pulp, which create the painful sensation. When cold, heat, spicy food or a dental instrument touches the bare dentin on the root of the tooth, fluid moves in the dentin tubule and the mechanotransducer in the pulp creates a painful signal.
- 4. is GERD really a major cause of recession? what are the strongest correlates? always assumed age was the strongest
Ian Furst (talk) 17:19, 22 December 2013 (UTC)
- OK, I will put in refs now
- Agree. This content needs to be added to dentin hypersenstivity at some point too. Perhaps on this article if we keep a pathophysiology seciton the hydrodynamic theory should go in there.
- I would prefer not to use the phrase "sensitive teeth". As you ofc know, all healthy teeth are sensitive. "Sensitive teeth" is a term used by oral hygiene companies to sell desensitizing toothpastes. I see TV ads where someone has been "successfully treated for sensitive teeth" and now he can happily chew and crunch on ice cubes. This is nonsense, it is normal and healthy to experience some sensitivity from the teeth if you eat an ice cube. If anything, now he has hyposensitivity. Yet another example of manipulation of the public's mindset to believe that they are unhealthy, or will become unhealthy if they do not buy some product of questionable efficacy.
- Apologies, I did not intend to suggest GERD causes gingival recession. To clarify, GERD may cause acid erosion, but not recession. Lesion (talk) 19:52, 22 December 2013 (UTC)
Good point re: sensitive teeth, my only concern being that 99% of the lay public will not draw the connection between "sensitive teeth" and "dentin hypersensitivity", imo and go along believe sensitivity to biting on an ice cube is abnormal. I think it would be better if you use a more formal version of point #3, maybe after reference #19? Something like, "This is sometimes referred to as sensitive teeth, however, truly sensitive teeth will.... whereas normal healthy teeth experience......". Right or wrong, the connection will exist in the minds of most, better to correct they myth than to avoid? Also, all but 1 of the references used are primary and I think could be replaced from most textbooks (e.g. nothing cutting edge being mentioned). Is there are particular reason you used them? Ian Furst (talk) 22:57, 22 December 2013 (UTC)
- Might be an idea... that extra sentence would make this point well. Which is the primary source? I thought it was already removed (Li200X)? If I have used a primary source yes we should replace it with secondary or textbook. Lesion (talk) 23:12, 22 December 2013 (UTC)
- I might be mistaken here, are general lit. reviews considered secondary? Thought they had to be systematic reviews or meta-analysis. Also, noticed a couple where the same article quoted multiple times (using {{cite pmid||, for articles (where all the page numbers are the same) its worth while to give them a ref name Ian Furst (talk) 01:43, 23 December 2013 (UTC)
Forgot: this sentence, "Most researchers concur that the pulp is notusually inflamed in this condition, and that nerves in the pulp have not become more sensitive to stimulae,[21][22] but rather that the stimulae have become more intense due to loss of insulating layers of tissues that used to separate dentin from the external environment. ". Doesn't read very well. It has a lot of qualifiers in it (most researchers..., not usually...,)and the point has already been made when you talk about the loss of cementum, enamel and gingiva. I was going to RW but I think the paragraph stands without it, unless there's a particular point you think has not been made? Ian Furst (talk) 23:05, 22 December 2013 (UTC)
- OK remove that sentence if you think best. People can always go and read more in detail on the main article ... we only need to provide a short summary focusing on the toothache aspect of each condition... Lesion (talk) 23:12, 22 December 2013 (UTC)
- found the definitions for primary, secondary and tertiary sources at Wikipedia:MEDRS for my own reference. Reviews are considered secondary. sorry about that. Ian Furst (talk) 01:36, 29 December 2013 (UTC)
Work to resume
I have been wrapping up a publication in last few days. Sending to journal today so should be back on this task soon.
If you are interested, I was thinking to eventually get this article to GA and then publish it via that method for wikipedia articles (I sent you the link after you wrote dental implant if you remember). I know this goal would help motivate me. Lesion (talk) 13:20, 1 January 2014 (UTC)
- sure, I'm hoping that things will slow down for me a bit in January and I could devote more time to it. I didn't realize that the publication project had gone forward - I'd assumed it was just an idea. I'd appreciate the ability to publish some of this. Have you gone thru the process yet? Does it work? When peer review happens, how do they handle the more laid-back layperson language of Wikipedia compared to an academic resource (e.g., are we going to have to reword the entire project to appease the journal's editorial/copyright staff?). Ian Furst (talk) 15:49, 1 January 2014 (UTC)
- To clarify, I have not published through wiki before... this other publication was off wiki. Proposing to publish toothache or orofacial pain to see what it is like with JMIR Wiki Medical Reviews. Lesion (talk) 17:42, 1 January 2014 (UTC)
Pathophysiology section
I have moved this section to immediately follow the lead. This is not the MEDMOS, but I think it works better for this particular article. Suggest put into this section:
- Definitions
- Basic anatomy, including what type of pain fibers are present in the different tissues. Lesion (talk) 15:12, 25 December 2013 (UTC)
We are mentioning the spread of odontogenic infection several times. We should probably only mention it in one place. Not sure if it is better to do this in the "pathophysiology" section or the "prognosis" section... Lesion (talk)
- starting to work on this, agree with the definitions and basic anatomy and can add infectious. Because the specific path is discussed in each of the differential diagnosis sections, I think I'll do a blurb on bacterial, chemical, trauma, etc... causes. These two paragraphs's,
Dental causes of toothache tend to be considered as either pulpal or periodontal. The teeth and the periodontium (i.e. the tissues that support the teeth) are innervated by the maxillary and mandibular divisions of the trigeminal nerve. The maxillary (upper) teeth and their associated periodontal ligament are innervated by the superior alveolar nerves, branches of the maxillary division, termed the posterior superior alveolar nerve, anterior superior alveolar nerve, and the variably present middle superior alveolar nerve. These nerves run through the maxilla in close relationship with the maxillary sinus before together forming the superior dental plexus above the maxillary teeth. The mandibular (lower) teeth and their associated periodontal ligament are innervated by the inferior alveolar nerve, a branch of the mandibular division. The inferior alveolar nerve enters the medial surface of mandibular ramus at the mandibular foramen and runs inside the mandible, below the mandibular teeth in the inferior alveolar canal giving off branches to all the lower teeth (inferior dental plexus).[2][3]
The oral mucosa of the gingiva (gums) is also innervated by branches of the trigeminal nerve, however often the gum will be innervated by a different nerve to the adjacent tooth. The gingiva on the facial (labial) aspect of the maxillary incisors, canines and premolar teeth is innervated by the superior labial branches of the infraorbital nerve. The posterior superior alveolar nerve supplies the gingiva on the facial aspect of the maxillary molar teeth. The gingiva on the palatal aspect of the maxillary teeth is innervated by the greater palatine nerve apart from in the incisor region, where it is the nasopalatine nerve (long sphenopalatine nerve). The gingiva of the lingual aspect of the mandibular teeth is innervated by the sublingual nerve, a branch of the lingual nerve. The gingiva on the facial aspect of the mandibular incisors and canines is innervated by the mental nerve, the end branch of the inferior alveolar nerve after it emerges from the mental foramen of the mandible. The gingiva of the buccal (cheek) aspect of the mandibular molar teeth is innervated by the buccal nerve (long buccal nerve).[3]
- seem like too much info for this article. I'd like to limit the talk on the anatomy of the trigeminal nerve to V-2 and V-3, and leave the specific stuff to the actual articles on the subject. What are your thoughts on it? Ian Furst (talk) 15:21, 27 December 2013 (UTC)
- Yes OK I will reduce those paragraphs. I think the main question we should ask ourselves at this point is: Do we want a pathophysiology section, or should we discuss these things as we go along in the differential diagnosis section? I tend to favor having a pathophysiology section as many concepts apply to several different types of toothache that we will discuss in the ddx section. It just looks pretty messy atm. This is why I put a "Don't read this article right now" sign on the top =D Lesion (talk) 15:55, 27 December 2013 (UTC)
I've been searching around for a comparable that has reached good article status, chest pain, back pain, headache and abdominal pain are all mostly lists. But check out Low back pain, reads well, good balance of diagrams and it's reached good article status. The biggest thing, is that the sections don't follow the classic MEDMOS guidelines and use everyday language.
My suggestion would be to promote the differential diagnosis section and rename to causes. Demote the pathophysiology section and shorten to a 1 paragraph section which includes the current first paragraph and a short synopsis of para 2 and 3 (e.g. the innervation). With subcategories of pathophys of anatomic structures (tooth, bone, muscles) and pain pathways (innervation).
Our categories could be opening, causes, pathophysiology, diagnosis, management (I liked this term more than treatment, it saves us from having to write a dissertation on rct, pulpectomy, etc..., instead we can give a quick blurb for each and point to the proper article), prognosis then leave the rest the same?
Are you re-doing pathophys? I thought I was going to deal with that one - or have you already launched into it? Tell me a subsection you're not working on so that I can. Also, great call on the diagram - been following the conversation over there and it looks like it will be a winner. Ian Furst (talk) 02:10, 28 December 2013 (UTC)
- Hi Ian (gah, I've been on Wiki too much today). Started earlier but then got distracted by various Wikidramas. Yes pathophysiology section probably needs to be more focused. What do we need to discuss in this section? Funny you should mention low back pain, written by an experienced editor zad68. I already was planning to ping him/her when we had more to show here and see what we could learn from low back pain. Rationale for moving pathophysiology section to first was that it discussed many issues that would later be needed throughout article. Please feel free to switch back if you don't feel it is working. Happy to use management instead of treatment. Agree we should not go into detail about any individual treatment, but might be worth quick mentions about how interventions impact on toothache? E.g. how long will the pain last after an extraction or RCT etc. Agree with your proposed structure of management section. Please feel free to work on any section... no need to divide them between us... Lesion (talk) 02:23, 28 December 2013 (UTC)
- K, I'm going to move and rip apart pathophys - will find some way to make it flow (tomorrow morning). Thx. Ian Furst (talk) 02:35, 28 December 2013 (UTC)
- cleaned and compressed, removed the path of trigeminal, my logic being that the discussion (while it obviously took a lot of work to create), didn't really add a lot to the understanding of toothache. When I chopped it out, the section was simpler to read and imo still gave the same info wrt pain. Ian Furst (talk) 16:58, 28 December 2013 (UTC)
- OK. I have a feeling there is another article that might benefit from that section about innervation of the teeth and gums... maybe an anatomy one? Lesion (talk) 22:19, 28 December 2013 (UTC)
- Moved that content to Human mouth, which also is a little neglected I notice. I am looking again at this article and I find the state of the references distressing, is there no way we can tidy these? Lesion (talk) 01:13, 3 January 2014 (UTC)
- OK. I have a feeling there is another article that might benefit from that section about innervation of the teeth and gums... maybe an anatomy one? Lesion (talk) 22:19, 28 December 2013 (UTC)
- cleaned and compressed, removed the path of trigeminal, my logic being that the discussion (while it obviously took a lot of work to create), didn't really add a lot to the understanding of toothache. When I chopped it out, the section was simpler to read and imo still gave the same info wrt pain. Ian Furst (talk) 16:58, 28 December 2013 (UTC)
- K, I'm going to move and rip apart pathophys - will find some way to make it flow (tomorrow morning). Thx. Ian Furst (talk) 02:35, 28 December 2013 (UTC)
Expansion
I suggest the WP:MEDMOS recommended headers for signs/symptoms. Might not be able to find any content for some of the sections. Also, I merged History with society and culture.
Essentially, since this is a symptom, I suggest a glorified list format. The differential diagnosis section might constitute the majority of the article, with a short paragraph linking to each cause and giving a brief description. Diagnostic approach could do with major expansion. Not sure what could go into pathophysiology. Talking about innervation and pain fibers maybe? Lesion (talk) 16:29, 14 December 2013 (UTC)
==Differential diagnosis==
===Pulpitis==
Pulpitis is inflammation blah blah...
===Cracked cusp syndrome===
(←Also we maybe need to make this stub, not sure how it is different to cracked tooth syndrome or if they are the same thing)
... etc
Definition of toothache?
I think we should keep focussed on pain felt in the teeth, gums and/alveolus on this article. I consider toothache to be a specific type of orofacial pain, which may include other parts of the face...
Some of the definitions of toothache I am reading in popular online dictionaries I do not feel are suitable:
An aching pain in or near a tooth.
...but not all pain felt in teeth is aching in character.
An ache localized in or around a tooth.
...same as above. Also not all pain felt in teeth is localized.
A pain in or about a tooth.
...better, but what about radiation?
The definition we are using right now is made up by me, but I am still not happy with it. We use "pain" instead of "ache", and we say "one or more teeth" instead of referring to a single tooth. After all, someone with bruxism or TMD might complain of "toothache" in several teeth. Should we add the qualifier "which may be well localized or poorly localized"? Should we add "which may radiate to other parts of the face"? Lesion (talk) 16:42, 14 December 2013 (UTC)
- perfect start, whenever I talk about orofacial pain (TMD, etc...) I always lead with the fact that toothache is the most common cause of orofacial pain. Based on that, toothache becomes a descriptor for the etiology of pain not a locator. It's like the difference between chest pain (location), cardiac pain (etiology), pain of myocardia ischemia (pathologic cause). In this case; orofacial pain, toothache, pulpitis. To that end, we should not limit toothache to location or pathologic cause (we can discuss each in the detail?) but discuss it as a specific type of pain. Maybe something like, "toothache is unpleasant sensory and emotional experience associated with actual or potential tissue damage of the tooth and it's supporting structures". This is a direct play on the definition of pain.Ian Furst (talk) 20:54, 14 December 2013 (UTC)
- crap; didn't bother to read the definition you'd already done at the top (just the ones you got from the web). As an FYI, whenever I post, it's always intended as a suggestion to be critiqued and, if need be, ripped apart. Please excuse if I fail to post it as a suggestion, sometimes my typing and brain get ahead of my manners. As for the definition, "Toothache is pain felt in one or more teeth, the periodontium (gums) and/or the alveolus." works well. I wouldn't add any qualifiers as to location. My two critiques would be a) "felt 'in the..." limits location, whereas we want to limit causation(?) and b) "the periodontium (gums) and/or the alveolus." is too scientific for the layperson as part of the definition. In my mind, a layperson should be able to read and understand the definition by itself in wikipedia. What do you think about, "Toothache is pain caused by actual or potential damage to the either the teeth, their supporting structures or both." Ian Furst (talk) 21:22, 14 December 2013 (UTC)
Chest pain → cardiac pain → MI : Orofacial pain → toothache → pulpitis. Yes excellent analogy. Agree with you about not limiting toothache to one presentation or etiology. It is a very general term. Perhaps we are overthinking things. Imo, it is entirely appropriate to list all the potential etiologies of toothache on this page, but we will have dedicated pages for nearly all of them (except for specific descriptive things like "food packing"). It would be good to have a definition of pain early in the article.
I am not happy with my current definition. I added "felt in" because this covers "nonodontogenic odontalgia" e.g. referred pain from the maxillary sinus which is perceived in the teeth.
I like parts of your wording.
"supporting structures" avoids jargon like alveolus.
But "actual or potential damage" does not cover referred pain or atypical odontalgia etc etc. I would like to get across in the definition that rarely there is no disease of the teeth or supporting structures.
How about this:
Toothache is pain perceived as originating in a tooth (or multiple teeth) and/or the supporting structures (i.e. the periodontium). Very commonly, toothache is caused by some disease process of the teeth or gums; but rarely other conditions can cause toothache without any evident dental cause, e.g. referred pain from maxillary sinusitis.
"Perceived as originating" hopefully does not limit the location, and includes radiating pain. I think it would be good to say "single or multiple teeth" if not "which may be well localized or poorly localized". Suggest giving maxillary sinusitis as the nonodontogenic odontalgia example in the lead. I believe it is the most common non dental cause, but I have no source. It has been said that TMD pain is the second most common cause of orofacial pain, but per your analogy above, TMD pain may not always be toothache. Lesion (talk) 21:52, 14 December 2013 (UTC)
- Good point re sinusitis; causes toothache without causing pathology in the structures (or does it cause mild periapical pulpitis which causes the toothache?). Best to include a section of distant pathology that causes toothache, than to make the claim that toothache cannot be caused by non-odontogenic sources. The problem is toothache is pretty much self defining, but we need a succinct opening sentence for the article. I like what you cover. We should word-smith it down to a single sentence, rid it of adverbs and minimize the conjunctions. BTW, I have no reservation about overthinking the opening and especially the definition as it will set the tone for the rest of the article.
- The perceived part need not be added if we remove the causation part. Lets revert back a bit for ease of reading.
- How about,
Toothache is pain in a tooth or teeth caused by dental disease or localized non-dental disease that is referred to the teeth.
- I left out adverbs about frequency (commonly, less commonly) and the example to make it succinct. I figure the next two sentences in the lead paragraph can make those points. E.g., the next paragraph could be along the lines of, "...99% of toothace is caused by dental diseases, however....."Ian Furst (talk) 23:01, 14 December 2013 (UTC)
OK, I think we are getting there. I feel the wording "localized non-dental disease" might be confusing for readers? I also liked "supporting structures" that you suggested before. How about:
Toothache is pain in a tooth or teeth and/or supporting structures, caused by dental disease or non-dental disease which is perceived as toothache.
(Slightly off topic) When you ask about sinusitis causing mild periapical periodontitis, we are straying into the topic of maxillary sinusitis of odontogenic origin (aka odontogenic sinusitis), accounting for 10-40% of all maxillary sinusitis according to some reports. I think it is usually the other way around: the dental pathosis causes inflammation of the membrane of the sinus (see for example [4]). Perhaps sinusitis is a poor example (apart from being more common than the rest of the nonodontogenic toothaches), because the sinus is such an intimately related structure to the mouth, some sources do not consider this to be true referred pain. This is a quick excerpt from a paper I wrote recently:
Maxillary sinusitis is not uncommonly perceived as pain originating in the maxillary molar and premolar teeth, which may trigger patients to seek dental care. This is an example of so called "non-odontogenic toothache".[14] In one report, 11% of patients with sinusitis reported maxillary toothache.[15] In maxillary sinusitis, the posterior maxillary teeth may be tender to percussion,[16] and hypersensitive to cold stimuli. This is secondary hyperalgesia (i.e. concentric spread of pain beyond the area of tissue injury), rather than true referred pain.[17]
...Therefore "perceived as toothache" might be more general for the definition than specifically saying referred pain? Albeit incredibly rare, "percieved as toothache" also covers the truly psychogenic toothache. Lesion (talk) 00:29, 15 December 2013 (UTC)
- agreed, do you mind if we substitute the "and/or" with a longer sentence? Grammatically, I think it's technically allowed but is messy. See below; by using "the teeth" it allows one or many
Toothache is pain in the teeth, their supporting structures, or both; caused by dental disease or non-dental disease which is perceived as toothache.
Ian Furst (talk) 00:44, 15 December 2013 (UTC)
Just added a comma. I'm happy with this, not sure how others feel. Wonder if "in the teeth" should be "from the teeth" which better includes radiation of toothache into other parts of the face? Lesion (talk) 00:52, 15 December 2013 (UTC)
- Nah it's fine ... Lesion (talk) 00:53, 15 December 2013 (UTC)
- chicken and egg thing, we're discussing toothache which is, by intuitive definition, pain in the teeth. Referred toothache, might more properly be described as referred by from pulpitis (or whatever) as a type of orofacial pain. I think "in the teeth" is the more exacting description. Ian Furst (talk) 00:55, 15 December 2013 (UTC)
Diagnostic approach
would it be good to include a short list of all the common mistakes people make when diagnosing toothache? See for example Pericoronitis#Diagnosis E.g. the "migratory abscess", where a pericoronal abscess tracts along the buccal sulcus and forms a parulis over the buccal aspect of the 6, and the 6 is extracted accidentally. Or diagnosing bilateral toothache in the lower posterior region as bilateral pericoronitis when in fact the myofascial element is more responsible for the pain. I'm also thinking about poorly localized toothache leading to treatment of a nearby obvious problem which is not contributing to the pain, when in fact there is some root caries in a periodontal pocket on the causative adjacent tooth. I have come across this sometimes. The grossly broken down tooth is dead and is not causing any of the pain, but the adjacent vital tooth with the tiny bit of decay is causing all the pain.
A few examples might highlight to readers how difficult it can be sometimes to diagnose the cause of toothache, even if that cause is dental and we are not looking at nonodontogenic toothache. Lesion (talk) 22:28, 14 December 2013 (UTC)
- agree, I think the practical way to approach this may be in the diagnostic section, talking about each sign/symptoms/test and how it might be interpreted (including in there the potential for the wrong diagnosis). I'm thinking we might use the "signs and symptoms" template from MEDMOS
- What about a table giving the Socrates (pain assessment) parameters for the main types of toothache (reversible pulpitis, irreversible pulpitis, acute periapical periodontitis, periodontal abscess, acute pericoronal abscess, myofascial pain)? See for an example what I did on pages like burning mouth syndrome. Here is roughly what I mean below (not thought too much about content, just an example). Lesion (talk) 21:32, 16 December 2013 (UTC)
| Parameter | Dentin hypersensitivity | Reversible pulpitis | Irreversible pulpitis | Acute periapical periodontitis/ periapical abscess | Periodontal abscess | Pericoronal abscess | Myofascial pain | Maxillary sinusitis |
|---|---|---|---|---|---|---|---|---|
| Site | Poorly localized | Poorly localized | Poorly localized, unless combined with periapical periodontitis | Well localized. Classically patient able to point to involved tooth | Usually well localized | |||
| Onset | - | - | - | |||||
| Character | Sharp, shooting | Dull, continuous pain. Can also be sharp | Dull, continuous throbbing pain | Dull, continuous throbbing pain | ||||
| Radiation | Does not cross midline | Does not cross midline | Does not cross midline | Does not cross midline | ||||
| Associated symptoms | Patient may complain of receding gums and/or toothbrush abrasion cavities | - | - | Tooth may feel raised in socket | ||||
| Time pattern | Hypersensitivity as long as stimulus applied. Often worse in cold weather | Pain as long as stimulus applied | Shooting pain when stimulus applied, but pain continues after stimulus removed. Also spontaneous pain with no stimulus. | |||||
| Exacerbating/Relieving factors | Exacerbating: thermal, particularly cold | Exacerbating: thermal, sweet. | Simple analgesics have little effect | May still show symptoms of irreversible pulpitis, or no response to cold stimulus (pulp necrosis). Pain on application of heat may be more of a feature. Lying down worsens pain due to increased local blood pressure. Hurts to bite on tooth | ||||
| Severity | Less severe than pulpitis | Severe, for short periods | Severe | Severe | ||||
| Effect on sleep | None | None usually | Disrupts sleep | Disrupts sleep |
- love it. If you work on that, i'll do the narrative for the ddx section. I don't have a lot of basic textbooks left (but do have stuff like pathways of the pulp, etc...) so may need some help with referencing later.Ian Furst (talk) 01:18, 17 December 2013 (UTC)
- I found a source for some of this content:[2] click look inside then search for "toothache". A slightly different table is on p70.
- Re textbooks, most of the sources listed in User:Lesion#Sources I have in pdf. I am happy to share via dropbox. Currently I have Carranza's clinical periodontology [3] and Lindhe Clinical periodontlogy and implant dentistry [4]. If you want any others let me know and I will see if I can help. Lesion (talk) 11:17, 17 December 2013 (UTC)
Symptoms or signs
Most articles about medical signs and symptoms should follow the below recommended structure. Omit sections that your sources do not address and combine sections when this seems sensible. For example, the definition of some signs is amply covered by an explanation of the mechanism, so having a section dedicated to the definition would be redundant.
- Definition (current definitions)
- Differential diagnoses or Associated medical conditions
- Pathophysiology or Mechanism
- Diagnostic approach or Evaluation
- Treatment or Management (for the symptom itself, if any: e.g., analgesics for pain)
- Epidemiology (incidence, prevalence, risk factors)
- History (of the science, not of the patient: e.g., "The oldest surviving description is in a medical text written by Avicenna.")
- Society and culture (e.g., cachexia was a literary symbol for tuberculosis in the 19th century and for AIDS in the 1980s.)
- Research (Is anything important being done?)
- Other animals
- Agree. Not sure we will find anything about other animals and research. This structure is what we have currently, although I merged "history" and "culture and society" mostly because I was feeling a bit brain dead and didn't feel like separating the content going in there. Lesion (talk) 00:58, 15 December 2013 (UTC)
differential diagnosis for pulpal conditions
Lesion - I was hoping to convert the existing lists into a narrative that is more user friendly. Here is a draft (without any links or references yet) I've been working on for pulpal conditions. What do you think about it? My thought, is that if you like the general tone, we can edit this paragraph together to get a better sense of each other's editorial style, then (assuming we find common ground) divide the remaining paragraphs.
The most common cause of toothache is pulpal inflammation. Each tooth is made of enamel over a softer core called dentin. Under the dentin, on the inside of the tooth, the root canal and pulp chamber contain the nerves and blood vessels of a tooth. The pulp structure is soft tissue (compared to the hard tissue of the outer structures) and susceptible to inflammation. When the pulp of the tooth becomes inflamed, a pulpitis occurs, nerves become sensitized and a toothache occurs. Many things can cause pulpitis such as cavities, a cracked tooth, a leaking filling and trauma.
Inflammation and swelling of the pulp cause sensitivity to cold and sometimes hot. If treated early or if the insult to the pulp is mild, the inflammation subsides, and the symptoms disappear. This is called reversible pulpitis and is usually characterized by short lasting pain to cold. If the pulp swells too much, however, the swelling constricts the vessels at the end of the tooth root and can obstruct the blood supply. The pulp in the root canal and chamber will then die. This type of inflammation is called irreversible pulpitis and is similar in principal to the swelling that occurs in a brain injury. The hallmark of irreversible pulpitis is spontaneous pain or lingering pain to cold. Once the pulp completely dies, there can be a period when the tooth doesn’t hurt unless it is causing periapical periodontitis. After that, the dying tissue, bacteria and gases build up in the pulp chamber and can force their way through the apex of the tooth. During this time, tooth pain is spontaneous and the tooth becomes tender to bite on as the periapical tissues inflame. Hot drinks can make the tooth feel worse (it's speculated that gases inside the pulp chamber expand), likewise, cold can make it feel better. The dental pulp is now necrotic and emergency treatment is required.
Ian Furst (talk) 14:19, 16 December 2013 (UTC)
- I got distracted by periodontal abscess yesterday. Back on task here now. By the way, I am happy for you or anyone else to place their edits directly into the article. No need to get things "approved" on talk page first. I don't own this article. Yes definitely agree to convert the brief list we have into narrative. In fact I already started to do this, by making "pulpitis" into its own section. You asked for feedback about this wording, so:
- We want a clear and concise discussion of pulpitis, because we have already a dedicated article on pulpitis.
 Done
Done - This section should focus on how pulpitis causes toothache, and how the toothache is different between reversible and irreversible pulpitis.
- "Deep to the dentin" -- consider instead "underneath the dentin"
 Done
Done - Suggest mention that the pulp and root canal system is filled with soft tissue, to contrast with hard tissues enamel and dentin
 Done
Done - Might be worth mentioning that stroma of pulp is rather fibrous, and it is soft tissue contained within an inexpandible hard tissue "box". Therefore, it has no space to expand when it gets swollen. Compare with compression syndrome
 Done more analogous to increased ICP so drew that parallel.
Done more analogous to increased ICP so drew that parallel. - "cause cold sensitivity"-- I would say "thermal" to cover hot as well, and mention sweet. Possibly mention mechanism pulp hydrodynamic theory (can't remember).
 Done "cold and sometimes hot" since cold is more common - hill look up mechanism - waiting on textbook pathways of the pulp from a friend
Done "cold and sometimes hot" since cold is more common - hill look up mechanism - waiting on textbook pathways of the pulp from a friend - Necrotic pulp-- yes worth mentioning that once pulp is dead, there may be sudden relief of pulpitis pain. Unless already acute periapical periodontitis ofc.
- "force their way through the apex of the tooth. During this time, tooth pain is spontaneous and the tooth is tender to bite on." -- this is periapical periodontitis, not pulpitis... Pulpitis alone is not tender to bite or tender to percussion. Pulpitis alone is usually poorly localized.
 Done
Done
The think most logical way to organize discussion of causes is:
- Odontogenic toothache
- Pulpal pain
- Periodontal pain
- Nonodontogenic toothache
- "hot [...] expand the gases" -- I wonder... is the heat increasing the blood flow, and hence the pressure. Is there any gas trapped, or is it liquid, e.g. pus. Sometimes patients find that placing a hot water bottle on their face soothes the pain of a dental abscess. However, heat also draws the infection out. Placing heat on the face may encourage a cutaneous sinus, so I always tell people not to do this. Not sure how you feel about this. I will look for a source. Lesion (talk) 18:05, 16 December 2013 (UTC)
 Done I don't think it can be bloodflow, most of the cases can be opened without local and there's no blood what-so-ever. Will look for a source too Not a believer that hot will create a sinus - in my carrier I've seen 1/2 dozen cutaneous sinuses and they only form after years of neglect but that's just anecdotal opinion. Ian Furst (talk) 17:48, 20 December 2013 (UTC)
Done I don't think it can be bloodflow, most of the cases can be opened without local and there's no blood what-so-ever. Will look for a source too Not a believer that hot will create a sinus - in my carrier I've seen 1/2 dozen cutaneous sinuses and they only form after years of neglect but that's just anecdotal opinion. Ian Furst (talk) 17:48, 20 December 2013 (UTC)
- K - will make some changes and post to the page. Had no intention of approving everything on the talk page, but wanted to get a handle on your writing style before overhauling 1/2 the article one way, only to have you do the other in a different style. If you're on-board with the stylistic bent of this, I'll make some changes (tonight/tomorrow), we can edit the hell out of this then make some decisions about how to divide & conquer the remainder. Sound like a plan? Ian Furst (talk) 18:36, 16 December 2013 (UTC)
citation format
Hey Lesion, part II of today's missives. As we start to build this, what do you think about using the {{cite|pmid}} and {{cite|isbn}}? That way, as we build other articles we should have a mass of books already referenced in global templates? I've been using it in the dental implant and also find it helps with readability in edit mode. Ian Furst (talk) 14:38, 16 December 2013 (UTC)
- OK. I haven't used this method of citing before. I worry that the bot will fill out the fields with format errors, but it seems to have handled the refs on dental implant with no issues. Lesion (talk) 20:59, 16 December 2013 (UTC)
- you get used to it fast, plus it makes citing the same textbook with different pages a lot easier because you don't have to remember what you tagged the book with, just insert the isbn. Also, the autofill bot only works on {{cite|pmid}} for {{cite|isbn|| you fill it in one, on the template page then it's done forever (no matter what article it's used in). Ian Furst (talk) 01:21, 17 December 2013 (UTC)
- I'm finding this method confusing, but I have been using it since you posted this message. Ideally all the references in an article should be in the same format. Q= when you say just put hte isbn, so I do not need to put "ref name=" if I want to use a source more than once? Lesion (talk) 13:40, 20 December 2013 (UTC)
- you get used to it fast, plus it makes citing the same textbook with different pages a lot easier because you don't have to remember what you tagged the book with, just insert the isbn. Also, the autofill bot only works on {{cite|pmid}} for {{cite|isbn|| you fill it in one, on the template page then it's done forever (no matter what article it's used in). Ian Furst (talk) 01:21, 17 December 2013 (UTC)
correct for {{cite isbn| xxx|pages=a-b OR page=zz}}, essentially it creates a unique template page for that book. Every time it's cited, it just grabs the info from the template page. The assumption is, you'll always be citing different page numbers anyways. However, if you want to cite the exact same reference twice (like you would with a PMID article or the exact same pages in a book) then you should include a refname. The only other different is PMID has a bot to autofill the template page, isbn does not. Ian Furst (talk) 23:27, 20 December 2013 (UTC)
- OK so that's textbooks. So if we wanted to cite the same pmid twice, would you just place the <ref>{{cite pmid|00000000}}</ref> again instead of ref name? Will this not generate a double listing in the reflist? I will figure this out soon, I've just been used to the other method... Lesion (talk) 00:05, 21 December 2013 (UTC)
The referencing is turning into a mess. Apologies if this is my fault, I am not used to this format. Lesion (talk) 15:06, 25 December 2013 (UTC)
- I have consolidated the 15 or so Pathways references into one entry. I am assuming that the 10e also could be used to support content sourced to the 8th ed, but I only have the former. The page range of the 8th ed was: [32,35-42], I do not know what it is in the 10ed.
- The original rationale to use this cite pmid /cite isbn does not make sense to me. It is harder to memorize a string of numbers than it is an author name. The more widely used method of citation is better imo, or maybe I have just been using the old way for too long and can't adjust to change. We should not have a mixture of citation styles in articles (some rule or guideline). In this article it was not working. We should also try and avoid using multiple editions of the same book, it is very confusing. Lesion (talk) 01:52, 3 January 2014 (UTC)
Orphaned references in Toothache
I check pages listed in Category:Pages with incorrect ref formatting to try to fix reference errors. One of the things I do is look for content for orphaned references in wikilinked articles. I have found content for some of Toothache's orphans, the problem is that I found more than one version. I can't determine which (if any) is correct for this article, so I am asking for a sentient editor to look it over and copy the correct ref content into this article.
Reference named "Neville 2001":
- From Bruxism: Neville BW, Damm DD, Allen CA, Bouquot JE. (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 21, 58, 59, 173. ISBN 0721690033.
{{cite book}}: CS1 maint: multiple names: authors list (link) - From Periapical periodontitis: Neville BW, Damm DD, Allen CA, Bouquot JE. (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 113–124. ISBN 0721690033.
{{cite book}}: CS1 maint: multiple names: authors list (link) - From Osteonecrosis of the jaw: Neville BW, Damm DD, Allen CA, Bouquot JE. (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. p. 746. ISBN 0721690033.
{{cite book}}: CS1 maint: multiple names: authors list (link) - From Temporomandibular joint dysfunction: Neville BW, Damm DD, Allen CA, Bouquot JE. (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 758, 759. ISBN 0721690033.
{{cite book}}: CS1 maint: multiple names: authors list (link) - From Pericoronitis: Neville BW, Damm DD, Allen CA, Bouquot JE. (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 73, 129, 133, 153, 154, 590, 608. ISBN 0721690033.
{{cite book}}: CS1 maint: multiple names: authors list (link)
I apologize if any of the above are effectively identical; I am just a simple computer program, so I can't determine whether minor differences are significant or not. AnomieBOT⚡ 02:17, 3 January 2014 (UTC)
- not sure how that got deleted - but it's my reference, will figure out how to add it back in this weekend. Ian Furst (talk) 02:25, 3 January 2014 (UTC)
- I deleted it, we had multiple references to the same textbook, I think different editions as with Pathways. Lesion (talk) 02:31, 3 January 2014 (UTC)
- I'm completely confused, normally I use (for example) the {{cite isbn|isbn=0721690033|pages=73,129}}, then fill in the template for the book. I only use the <ref name=Neville /> for textbooks if I'm citing the same exact page. What'd I do wrong - not sure what the bot is telling us. Ian Furst (talk) 15:37, 3 January 2014 (UTC)
- There is nothing wrong with that reference style, or so I understand. For example, your referencing technique on dental implant, where the same source appears multiple times, is fine. However, on this page we had a mixture of referencing techniques and it was driving me nuts. I looked up WP:CITEVAR which said should not have different citation styles on the same article. Therefore, I made a arbitrary decision to convert the article to a single style. In doing this, I consolidated the 2-3 duplications of the source "oral and maxillofacial pathology" by Neville et al. However, the named reference stored on the page was <ref name=Neville2001 /> and I accidentally invoked <ref name="Neville 2001" />. Note space and quotation marks. Hence, the reference did not translate, and this is auto flagged to this bot. The bot then looks around on other articles to see if it can find another stored named reference of the same name. Since it found several, all with different page ranges, it posted a message here asking which reference to use. To fix this problem, I changed the incorrect "Neville 2001" to Neville2001. This problem is fixed, so we can ignore the bot. Hope that explains things... Lesion (talk) 16:29, 3 January 2014 (UTC)
- I'm completely confused, normally I use (for example) the {{cite isbn|isbn=0721690033|pages=73,129}}, then fill in the template for the book. I only use the <ref name=Neville /> for textbooks if I'm citing the same exact page. What'd I do wrong - not sure what the bot is telling us. Ian Furst (talk) 15:37, 3 January 2014 (UTC)
- I deleted it, we had multiple references to the same textbook, I think different editions as with Pathways. Lesion (talk) 02:31, 3 January 2014 (UTC)
Tooth labels

looking for input on which labels to add, will do it as numbers (so legend will go underneath). Because this is a general article, I wasn't going to go crazy with the labels, just those needed to explain toothache. Here's what I thought (each will be a number):
- crown
- root
- enamel
- dentin & dentin tubules
- pulp chamber
- blood vessels & nerve
- periodontal ligament
- apex
- alveolar bone
Ian Furst (talk) 19:34, 3 January 2014 (UTC)
- Sounds good. Consider "Apex" label as we talk about apical periodontitis in this page? Lesion (talk) 20:50, 3 January 2014 (UTC)
Pictures for diagnostics
I've taken high quality pics of tooth sleuth, ethyl chloride on cotton tipped applicator (cold), EPT, explorer/perio probe. Anything else I should get a shot of? Ian Furst (talk) 17:55, 10 January 2014 (UTC)
- Hi Ian. Apologies for lack of progress on my side, I have become distracted by other articles. Sounds very interesting re photos. These may well be useful on several articles not just toothache. Other things I can think of might be a radiograph of a GP point in a sinus to indicate the causative tooth, perhaps also a picture of a tooth with cracked tooth syndrome or dentin hypersensitivity. These are long term.
- I must ask how you get consent from your subjects-- do you mention Wikipedia at all? I have always been too embarrassed to ask, but need to get over it, particularly when I have seen interesting things that should get photographed... Lesion (talk) 18:48, 10 January 2014 (UTC)
- Please never apologize for lack of progress, this is a marathon not a foot race. Walking away for a while also helps sometimes. I had a guy the other day for a sinugram and didn't even think about it - will get it (as well as others). I see, on average, 30 people a day so lots of opportunity. I have not yet crossed the bridge of showing any identifiable structure in any picture (I'm not sure how that consent process works on the Wikipedia side) but on my end, I explicitly ask the person and document it. We also have a blanket freedom of information form which states that we can use unidentifiable records for teaching. All are jacked that they're going to be "famous", or that they may help others. If I sense any hesitation (which is rare), I don't use it. It also seems insensitive to me in certain situations (e.g. cancers), so I just don't bother asking. The tooth sleuth (btw, check the diamond on the 1.4B; not from me) is a DA I work - she was happy to do it. I use a lightbox, macrolens and ring-flash for most of the equipment shots. All clinical shots in the implant article were taken as I was writing, everyone seemed amused that they'd be part of it. Ian Furst (talk) 22:21, 10 January 2014 (UTC)
vanity, body modification same as eyeball jewelry. It's just a diamond chip held on with composite, apparently an ex-employer did it for her. Pretty subtle Ian Furst (talk) 02:09, 11 January 2014 (UTC)
- Never saw such a thing. I wonder what the seal is like. Or will they end up with a nice diamond in the middle of a cavity... Lesion (talk) 02:34, 11 January 2014 (UTC)
- So far looks ok - I'm thinking decalcification similar to ortho brackets that stay too long. Doing a gif using the new diagram on the progression of pulpitis. Not sure how it will look yet, but thinking it's worth a try. Wiki needs a greater range of media imo. I assume the problem is that not everyone can edit a video, but this is pretty simplistic. Will see Ian Furst (talk) 02:52, 11 January 2014 (UTC)
Table
initial table filled in, will work on referring and rewording tonight/tomorrow - feel free to edit as well. It's a lot. Ian Furst (talk) 20:23, 14 January 2014 (UTC)
- lesion going to work on examination today/tomorrow - you mentioned something about bullet points, is the preference for bullet point (as is) or narrative? I've previously turned most sections into narrative but wasn't sure which is preferred. Ian Furst (talk) 01:55, 15 January 2014 (UTC)
is an online resource that a great many dentists around the world rely on for evidence based treatment decisions in dental trauma. It's a critical support but I can't fit it into any of the reliable sources pigeon holes. Any ideas? Leave it out?
rough draft
Hey Lesion, a rough draft of the completed article is now done imo. Some of the sections (perio abscess, occlusal trauma, part of necrosis) are still largely unreferenced. Next step is to read, start to finish for flow so you may see some copyediting. Will also watch to add pictures - don't like the endo pic so will get a new one. Ian Furst (talk) 11:48, 17 January 2014 (UTC)
dry socket
Should dry socket be classified under our periodontal pain? question from original author inline text. imo, including it in this article is arbitrary anyway (since there's no tooth, therefore no toothache) but should absolutely be included because it's so common. Periodontal seems a good a place as any, it's not non-dental, not pulpal. We could make another classification (for cysts, tumors, other diseases of the jaws that cause toothache) and include it in there? Ian Furst (talk) 22:09, 19 January 2014 (UTC)
- I put that hidden inline text because although one source gave dry socket as periodontal, I was not 100% sure this was accurate. We have several sources clearly stating that pulpal and periodontal are the 2 types of odontogenic toothache. If we take "periodontal" to mean "periodontium" this would include alveolar bone. After all, an apical abscess also involves the bone. The periodontal fibers are not gone once a tooth extracted, but the periodontal ligament tissue proliferates once the tooth is gone to colonize the stabilized thrombus. IMO, any pathology that has not directly arisen from the teeth is not odontogenic toothache, even if it is located next to the teeth in the alveolus. Then there are odontogenic cysts and tumors as you state above. Not sure what is best. Maybe another category "other" ? Lesion (talk) 22:38, 19 January 2014 (UTC)
::PoP, page 55 divides it into somatic and neural structures but then provides a more practical list for nonodontogenic sources,
- MSK
- neurovascular pain (otherwise known as headache)
- neuropathic pains (trigeminal neuralgia, etc...)
- psychological origin
- pain associated with pathologic structures
- This is all covered in non-dental sources of pain expect pathologic structures. Maybe we should divide the non-odontogenic section into Pain form the jaws and supporting structures (#1, #3, #5) and Pain from a distant source (#2, #4, cardiac, CNS pathology, throat and neck pathology). What do you think? Ian Furst (talk) 00:42, 20 January 2014 (UTC)
I went to the subsection with the intent of reorganizing, but I think it reads well and hits all the highlights mentioned about. Agree that DS should be part of periodontal. Ian Furst (talk) 02:11, 20 January 2014 (UTC)
prognosis section
started reading thru the prognosis section to insert references and realized it deals mostly with a description of the naturally history of pulpitis. I was think the section should deal more with the prognosis of the common conditions, if treated. thoughts? Ian Furst (talk) 20:54, 20 January 2014 (UTC)
- The natural history of pulpitis through to pulpal necrosis, periapicial periodontitis, spreading odontogenic infection/draining intra-oral sinus was not meant to be the only content in the prognosis section... agree should discuss both treated and untreated. Lesion (talk) 21:31, 20 January 2014 (UTC)
Awkward sentence, IMO
Awkward sentence, IMO; rewrite?
"At first, only noxious stimuli stimulate the nerve minimizing the pain felt to that time when the stimulus is applied (for instance cold)." --Hordaland (talk) 19:04, 26 January 2014 (UTC)
- Yes agree that's a lot of stimu-
- Initially, pain is only felt while a noxious stimuli is applied (e.g. cold). Lesion (talk) 19:20, 26 January 2014 (UTC)
Reworked innervation diagram
I felt old diagram placed too much emphasis on long buccal, mental and infraorbital nerves, none of which consistently supply the teeth. Lesion (talk) 19:33, 26 January 2014 (UTC)
Cold??
"Irreversible pulpitis, characterized by severe spontaneous pain and lingering pain to cold..."
Really? That's not my experience. I've had several root canals, and the pain preceding them was relieved, not intensified, by cold (ice in my mouth). --Hordaland (talk) 18:43, 26 January 2014 (UTC)
- You may have had periapical periodontitis rather than irreversible pulpitis at this stage... dental pain is difficult because one stage may overlap with the next and symptoms can vary... Lesion (talk) 19:14, 26 January 2014 (UTC)
- user:Hordaland you likely had pulp abscess, where the gases expand with hot (causing pain) and shrink with cold (relieving it). There was likely a period, 6-12mos prior to that, where the tooth was cold sensitive. That would have been the irrev pulpitis stage and the hot sens the abscess stage. Plus, the tooth doesn't always read the textbook :-) Ian Furst (talk) 20:05, 26 January 2014 (UTC)
Is it ready?
Hey Lesion, I think we've got it looking pretty good. Lots of pictures, all secondary sources (although the one trauma guide reference is still in, but also in the EL's). What are your thoughts about submission to GA? Ian Furst (talk) 20:13, 26 January 2014 (UTC)
- Please feel free if you wish... you did most of the recent work here. Lesion (talk) 20:15, 26 January 2014 (UTC)
- just looking for an opinion. Did you have area that you wanted to work on still? Plus, I've only submitted to GA once (and got shot-down), so I don't have a good feel for when an article is ready. Ian Furst (talk) 20:20, 26 January 2014 (UTC)
- are we still going to try submitting this for pulication?Ian Furst (talk) 20:21, 26 January 2014 (UTC)
- I understand first stage is getting to GA/FA. Yes I am happy to work more here and work towards that option. GA process on wiki is a bit hit and miss imo, very dependent upon who does the review... some editors are (much) more strict when interpreting the GA criteria, which I suppose is for the better in the end because there is a better article... Lesion (talk) 20:38, 26 January 2014 (UTC)
OK, I'm going to leave it alone for a bit and let you work your magic. Once you think it's ready for a GA submission, either let me know so I can help you make the changes as they're recommended or I can submit. Happy to help out either way. Like the additional cultural shots. Ian Furst (talk) 20:55, 26 January 2014 (UTC)
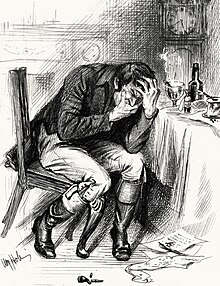
More society and culture images if required
-
The phrase "to complain of a toothache behind the ears" refers to fictitious pain complaint, as may be used by a malingerer. Detail from Netherlandish Proverbs (Pieter Bruegel, 1559).
-
Gargoyle with toothache on a medieval Anglican church (All Saints' Church, Holton cum Beckering, England).
-
Saint Apollonia, patron saint for sufferers of toothach, holds one of her own extracted teeth in a pair of forceps (Nuremberg Chronicle, Hartmann Schedel, 1493)
Could this be a better lead image? Lesion (talk) 13:25, 4 February 2014 (UTC) →
- ^ Hupp JR, Ellis E, Tucker MR (2008). Contemporary oral and maxillofacial surgery (5th ed.). St. Louis, Mo.: Mosby Elsevier. pp. 619–627. ISBN 9780323049030.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Cite error: The named reference
Grays2008was invoked but never defined (see the help page). - ^ a b Cite error: The named reference
Lindhe2008was invoked but never defined (see the help page). - ^ Shanbhag, S (2013 Jul). "Association between periapical lesions and maxillary sinus mucosal thickening: a retrospective cone-beam computed tomographic study". Journal of endodontics. 39 (7): 853–7. PMID 23791251.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help)







