Pelvic abscess
| Pelvic abscess | |
|---|---|
| Specialty | General surgery |
| Symptoms | High fever, pelvic mass, vaginal bleeding or discharge, lower abdominal pain[1] |
| Complications | Sepsis, peritonitis, fistula[1][2] |
| Causes | Gynecological surgery, abdominal surgery, pelvic infection, appendicitis, inflammatory bowel disease[1] |
| Diagnostic method | Blood tests, urine pregnancy test, blood and exudate culture, vaginal wet mount, medical imaging[1] |
| Differential diagnosis | Ectopic pregnancy, PID, appendicitis, kidney stone, bowel obstruction, sepsis following miscarriage[1] |
| Treatment | Antibiotics, drainage, adequate hydration[1] |
| Frequency | Uncommon[2] |
Pelvic abscess is a collection of pus in the pelvis, typically occurring following lower abdominal surgical procedures, or as a complication of pelvic inflammatory disease (PID), appendicitis, or lower genital tract infections.[1] Signs and symptoms include a high fever, pelvic mass, vaginal bleeding or discharge, and lower abdominal pain.[1] It can lead to sepsis and death.[1]
Blood tests typically show a raised white cell count.[1] Other tests generally include urine pregnancy test, blood and exudate culture, and vaginal wet mount.[1] Ultrasound, CT-scan or MRI may be used to locate the abscess and assess its dimensions.[1] Treatment is with antibiotics and drainage of the abscess; typically guided by ultrasound or CT.[3] Endoscopic ultrasound (EUS) is a minimally invasive alternative method.[3]
Signs and symptoms[edit]
Signs and symptoms include a high fever, pelvic mass, vaginal bleeding or discharge, and lower abdominal pain.[1] There may be urinary frequency, diarrhoea, or persistent feeling of needing to pass stool.[4] Other symptoms may include fatigue, nausea, and vomiting.[2] Clinical features might not be apparent until the pelvic abscess has grown in size.[2] The lower abdomen is generally tender; one or both sides.[2] A bulging of the front wall of the rectum might be felt on digital examination via the rectum or vagina.[2]
Complications include sepsis and peritonitis.[1] In the longterm, a fistula may develop.[2]
Cause and mechanism[edit]
Pelvic abscess typically occurs following gynecological surgery and abdominal surgery; hysterectomy, laparotomy, caesarian section, and induced abortion.[1] It may occur as a complication of pelvic inflammatory disease (PID), appendicitis, diverticulitis, inflammatory bowel disease (IBD), trauma, pelvic organ cancer, or lower genital tract infections.[1][3] The abscess may be in the pouch of Douglas, fallopian tube, ovary, or parametrium.[1] It begins as inflammation or a collection of blood in the pelvis.[1] Other risk factors include immunodeficiency, pregnancy, hydrosalpinx, endometrioma, poorly controlled diabetes, kidney disease, obesity, and genital tract abnormalities.[1][2] Opening the rectum to resect a rectal cancer may lead to developing a pelvic abscess.[3]
Females[edit]
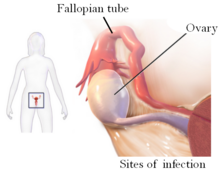
PID in females may lead to a tubo-ovarian abscess, where the abscess may be in the fallopian tube or ovary.[1][2]
Children[edit]
In children, it is more frequently associated with IBD and appendicitis.[5]
Diagnosis[edit]
Blood tests typically show a raised white cell count, often with a high ESR and C-reactive protein.[1] Other tests generally include urine pregnancy test, blood and exudate culture, and vaginal wet mount.[1] Medical imaging to assess the dimensions and locate the abscess may include ultrasound, CT-scan or MRI.[1]
Differential[edit]
Other conditions that appear similar include ectopic pregnancy, PID, appendicitis, kidney stone, bowel obstruction, and sepsis following miscarriage or termination of pregnancy.[1]
Treatment[edit]
Treatment is with antibiotics and drainage of the abscess; typically guided by ultrasound or CT, through the skin, via the rectum, or transvaginal routes.[3] Occasionally antibiotics may be used without surgery; if the abscess is at a very stage and small.[2] Until sensitivities are received, a broad spectrum antibiotic is generally required.[2] Sometimes, a laparotomy of laparoscopy is required.[2]
Endoscopic ultrasound (EUS) is a minimally invasive alternative method.[3] Treatment also includes adequate hydration.[1]
Further surgery such as is sometimes required to treat the underlying cause; such as salpingo-oophorectomy for tubo-ovarian abscess.[2]
Outcome[edit]
Pelvic abscess responds well to antibiotics and hydration.[1] The outcome is less successful in the presence of fistula.[2]
Epidemiology[edit]
It is uncommon.[2] The incidence of pelvic abscess is less than 1% in an individual undergoing obstetric and gynecological operative procedure.[3]
References[edit]
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z Khaliq, Khalida; Nama, Noor; Lopez, Richard A. (2022). "Pelvic Abscess". StatPearls. StatPearls Publishing. PMID 31424876.
- ^ a b c d e f g h i j k l m n o Tidy, Colin (23 July 2021). "Pelvic Abscesses". patient.info. Archived from the original on 16 March 2023. Retrieved 16 March 2023.
- ^ a b c d e f g Varadarajulu, Shyam (2022). "38. How to do EUS-guided pelvic abscess drainage". In Gress, Frank G.; Savides, Thomas J.; Casey, Brenna; Artifon, Everson L. A. (eds.). Atlas of Endoscopic Ultrasonography (Second ed.). Hoboken: John Wiley & Sons. pp. 182–185. ISBN 978-1-119-52300-0.
- ^ Saber, Alan A. (6 July 2022). "Abdominal Abscess Clinical Presentation: History and Physical Examination". emedicine.medscape.com. Archived from the original on 16 March 2023. Retrieved 16 March 2023.
- ^ Kyrazis, Crysta Iv; Rajderkar, Dhanashree (1 December 2022). "A Pictorial Review of Pelvic Pain-Beyond the Genitourinary System". Ultrasound Quarterly. 38 (4): 304–315. doi:10.1097/RUQ.0000000000000625. ISSN 1536-0253. PMID 36194672.
